Obesity in the Indian ocean region
The emerging embodiment of malnutrition
By Lauren Power
The World Health Organization (WHO) defines obesity as ‘a condition of abnormal or excessive fat accumulation in adipose tissue, to the extent that health may be impaired’; it is caused by a chronic positive energy balance. Obesity is measured using body mass index (BMI), a simple index of weight over height. An individual is considered to be overweight if they have a BMI equal to or over 25 and obese with a BMI of 30 and above.
While BMI is widely criticised as a measure, particularly for small-statured Asian populations, it remains the most useful population level measure, given available statistical information. Obesity is a leading cause of a number of non-communicable diseases. Overweight and obesity lead to adverse metabolic effects on blood pressure, cholesterol and insulin resistance. This increases the risk of coronary heart disease, stroke, diabetes, hypertension and several forms of cancer.
The economic transition towards higher levels of gross domestic product brings with it interconnected demographic, technological and nutritional transitions that have all contributed to the global rise in the incidence of obesity. The mechanisation, motorisation and computerisation of production processes since the beginning of the twentieth century, has resulted in increasingly sedentary lifestyles and decreases in the average energy expenditure needed for daily life.
Until the 1970s this decrease in physical activity was offset by a reduction in food energy intake. The 1970s saw an energy balance “flipping point” as energy intake rose in response to changes in global food systems. Changes in food production increased the supply of cheap, palatable and energy dense foods, while improved distribution systems made food more accessible and convenient; these changes were accompanied by more persuasive and pervasive food marketing. The time price of food decreased and total calorie production increased. High levels of state subsidies on agricultural production in the United States and Europe exacerbated the situation by prompting overproduction of subsidised staples, such as wheat, sugar and vegetable oils, pushing their prices to artificial lows.
Changes in global food systems have led to nutritional transitions as populations have shifted away from traditional diets towards globalised intake patterns, characterised by the consumption of energy dense, processed foods. Low and middle income countries have converged on a “western diet”, with high intake of refined carbohydrates, added sugars, fats and animal source foods.
Urbanisation is the major driving force behind nutritional transitions. Urban populations face heightened exposure to food marketing and greater availability of imported processed foods, through the presence of multinational supermarket chains and fast food restaurants. Lifestyle changes and greater involvement of women in formal labour markets, means less food preparation occurs in the home and more takeaway and street foods are consumed. Time spent in traffic and offices reduces energy requirements, while energy consumption increases. These factors partially explain why the incidence of obesity is higher in urban centres than rural regions in the developing world.
Diets that are heavy in energy dense, processed foods can meet daily energy requirements, while failing to deliver sufficient nutrients. The rapid transition of diets in the developing world has led to the emergence of “dual burdens” of nutrition in many countries, as obesity emerges as a health problem alongside undernutrition and micronutrient deficiencies. The dual burden exists not only at a country and community level, but can exist within households and even individuals, who may have both excess adiposity and micronutrient deficiencies.
Globalisation has increased the pace of these transitions; for developing countries, the nutritional transition is occurring earlier in the development process than it did in already developed countries, as they are exposed to altered global food systems. For instance, changes in production processes for edible oils have created an abundant supply of cheap vegetable oils that allow low and middle income countries to increase their energy consumption at very low income levels. Developing countries are thus gaining the health problems associated with overweight and obesity, before they have the public finance capacity to deal with them.
Obesity rates are increasing rapidly in the developing world, in part, because certain biological, cultural and institutional factors increase population susceptibility. Population physiology research suggests that the burden of obesity may be greater for much of Asia, Africa and the Middle East because of differences in fat patterning and body composition, and the cardio-metabolic effects of BMI at levels far below the standard BMI overweight cut-off. This increases susceptibility to NCDs at lower levels of adiposity. A complex interplay of biological factors operating during foetal and infant development also influences susceptibility to obesity and chronic disease later in life. Research demonstrates that foetal nutritional deficiency triggers anatomical, hormonal and physiological changes that enhance survival in “resource poor” environments. These developmental adaptations may increase the risk of obesity in subsequent environments with plentiful food resources.
Nutritional mismatch
Existing high rates of undernutrition in much of the Indian Ocean region may therefore influence the development and severity of the obesity pandemic. This nutritional mismatch is exacerbated in countries undergoing rapid social and economic development.
Cultural values may encourage the rise of obesity in some parts of the Indian Ocean region. Cultural preferences for small body sizes are dominant in the Western world and partially moderate drivers, such as increased food access. In parts of Africa, however, large body sizes are favoured and seen as a sign of good health and prosperity. Large bodies are also considered attractive in some Middle Eastern and South Asian cultures. This leads to a lack of awareness, as obesity is not seen as a problem but as an indication of high social status and health.
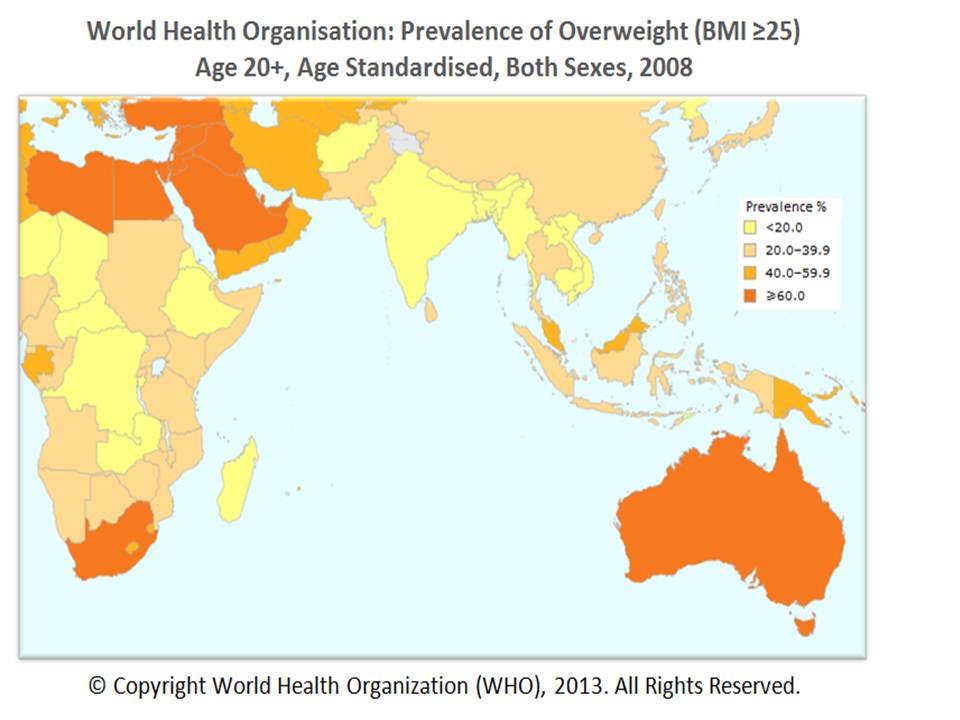
The incidence of overweight and obesity varies across high, middle and low income countries, but rates are overwhelmingly increasing throughout the Indian Ocean region. Obesity first emerged as a problem in developed and high income countries and it remains worse in these areas. Australia currently experiences one of the highest rates of obesity in the region; over 14 million adult Australians are overweight and over five million are obese. The prevalence of obesity has more than doubled in the past twenty years and it is now the single biggest public health threat facing the nation. The cost of obesity to Australia’s collective well-being is equivalent to around eight per cent of the economy’s annual output.
Obesity is also widespread in the oil-rich Gulf States of the Middle East. High income levels from oil production, and a heavy reliance on global markets for food supplies, have meant that Middle Eastern countries have imported the globalised consumption patterns that drive obesity rates. Bahrain, Saudi Arabia and the United Arab Emirates all have obesity rates of around 30 per cent. Kuwait has the highest global incidence, with almost 90 per cent of the population overweight and 35 per cent obese.
Overweight and obesity are rapidly emerging issues in low and middle income countries, which previously had very low prevalence of these conditions. As the pandemic of overweight spreads, developing countries in the Indian Ocean region face a double nutritional burden as obesity occurs alongside high levels of undernutrition. As economies develop and income levels rise, the risk of becoming obese is increasing across all socioeconomic classes, because of improved food access, the rise of sedentary lifestyles and the consumption of western diets. Rates of obesity are rising faster than they did in high income countries. In developing regions, high socio-economic groups in urban areas are the first to have a high prevalence of obesity; the burden shifts to lower socio-economic groups and rural areas as GDP rises. This shift is increasingly occurring at lower levels of development, as a result of the globalisation of food systems.
South East Asia has been experiencing rising obesity levels for over a decade, as its countries have undergone industrialisation and experienced rising income levels. Indonesia, Thailand and Myanmar all have levels of overweight between 20 and 40 per cent and have increasing problems with childhood obesity. Malaysia experiences the highest level of obesity in the region at 15 per cent.
South Asia has the lowest regional incidence of overweight and obesity; however, the conditions are rife amongst high income groups in India. Studies have shown that South Asians have a high tendency to store fat in the abdomen and organs, leading to a higher incidence of chronic diseases related to energy overconsumption at lower levels of adiposity.
Even in Sub Saharan Africa, which continues to face serious issues with undernutrition, obesity is on the rise, particularly amongst urban populations. With the exception of Madagascar, all countries on the East African seaboard experience an incidence of overweight between 20 and 40 per cent. Even in Madagascar, the incidence of overweight has risen significantly since the 1990s. The increase in obesity in Africa is predominantly occurring in cities and among new urban migrants. The rise in overweight is associated with poverty and food insecurity, as the urban poor are often unable to access or afford fresh and nutritious foods but must rely on cheap, energy-dense imports. The Lancet predicts that by 2030, up to 18 per cent of adults in Sub Saharan Africa may be obese.
Obesity is not yet as big a problem in the Indian Ocean region as hunger; however, it presents a potentially grave situation for future health and nutrition, as many countries in the region are experiencing rapid economic and social development. Without structural changes to food systems, obesity may continue to grow without the achievement of concurrent reductions in the incidence of undernutrition and micronutrient deficiency. Countries undergoing rapid economic and demographic transitions face the highest risk of developing obesity problems; this may lead to countries such as India and Indonesia, which are currently experiencing rapid growth, confronting large increases in obesity rates during coming decades. Rapid rates of urbanisation throughout the region are also likely to trigger rises in obesity. The burden of projected increases in global population to 2050 will predominantly fall on urban areas of developing countries. The urban population of developing countries is expected to double by 2030. This will expose increasing numbers of people to obesogenic environments.
The current health status of children in areas of South Asia and Africa is also an indicator of the magnitude of the forthcoming problem for the Indian Ocean region. Widespread child undernutrition will increase the susceptibility of future populations to overweight. Concurrently, the rising issue of childhood obesity in many states, particularly in the Middle East, foretells the extent of the issue, given the strong correlation between overweight in childhood and obesity later in life.
Limited fiscal capacity and the continued lack of recognition of the growing contribution of obesity to the burden of malnutrition in many regions will slow the implementation of food regulatory and nutritional awareness programmes, which could moderate the rate of growth in the incidence of overweight.
Implications for regional development
The rising incidence of obesity in the Indian Ocean region will have serious implications for public health, poverty, development and food security, at both the macroeconomic and household levels. Overweight and obesity are the fifth leading risk factor for non-communicable diseases (NCDs) and contribute to the incidence of the first and fourth leading factors, high blood pressure and high blood glucose. NCDs currently cause 80 per cent of deaths in low and middle income countries, with their prevalence expected to rise to 2030. Africa and South East Asia will be the regions hit hardest with increases of over 20 per cent by 2020.
Deaths caused by NCDs are predicted to rise by 60 per cent in South and South East Asia by 2030. Estimates for direct healthcare costs associated with obesity range between 2 and 8 per cent of total healthcare expenditure globally; this figure will increase as the obesity pandemic spreads to the developing world. Individuals who are obese incur medical costs that are, on average, 30 per cent higher than those of normal-weight individuals. The rising incidence of obesity-related NCDs will create a severe financial burden in developing countries in the region. It is unlikely that treatment could be accommodated within present health infrastructures and the majority of developing nations will not have the fiscal capacity to sufficiently expand the provision of health services. Africa is expected to suffer a double health burden as obesity puts pressure on health systems already strained by the high incidence of communicable diseases and conditions related to undernutrition.
In addition to these direct healthcare costs, overweight and obesity also incur considerable indirect costs for national economies. Studies undertaken in Europe and the US unequivocally demonstrate a negative association between obesity and work productivity. Being overweight inhibits physical function and increases absenteeism. It also decreases overall quality of life and life expectancy and creates social and psychological costs. In 2008, the annual cost of obesity to Australia, including health system costs and loss of productivity, was estimated at around AU$58 billion. Macroeconomic analysis has demonstrated that for every 10 per cent rise in the incidence of NCDs, the annual rate of economic growth falls by half a per cent.
The rise of obesity in the region poses a serious threat to national development. A reciprocal link exists between malnutrition and poverty, because of the relationship between nutrition and work capacity. Poverty exposes individuals to behavioural risk factors contributing to obesity and NCDs. By reducing an individual’s capacity to work, these factors become a driver of household poverty. WHO reports that each year, 100 million people are pushed into poverty because they have had to bear the cost of paying directly for health services. In Tanzania, where obesity levels are rising, especially amongst women, the cost of diabetes treatment is 25 per cent of the minimum wage. Obesity has the potential to weaken and even reverse progress in economic development, by reducing productivity and diverting resources towards healthcare. Predictions indicate that the rising incidence of obesity in the Indian Ocean region will impede poverty reduction initiatives.
In addition to healthcare and productivity costs, dietary energy overconsumption undermines food security on a global level. Current agricultural production is sufficient to meet total global consumption requirements, thus widespread obesity alongside undernutrition signals a failure of food distribution systems, which has led to obesity being classed as a form of food wastage. High demand for obesity-linked food products, such as sugar, vegetable oils and animal products, diverts water resources away from vegetable and grain production for human consumption.
One-third of global food production is used for the nutrition of livestock animals that contribute, at most, a quarter of total dietary energy supply; far less in most developing regions. Around two-thirds of agricultural land is devoted to this purpose, while only 8 per cent produces food for direct human consumption. While fuelling obesity, meat consumption diverts considerable resources away from forms of agricultural production that would enable greater improvements in food security; it also causes harmful environmental degradation.
Current distributional inefficiency in food systems means there is significant scope to reduce food insecurity by matching actual food needs with availability. By better aligning demand and supply, it is possible to improve food security without requiring large increases in agricultural production. Poor recognition of the public health issue confronting the Indian Ocean region because of rising obesity, however, means that the changes in consumption patterns necessary to improve food security and reduce malnutrition are unlikely to occur. Nutritional education and awareness campaigns and food quality and marketing regulations, such as front of package nutritional labelling, are limited or non-existent in most developing countries in the region. To an extent, there seems to be a lack of willingness to direct attention towards obesity in countries where it occurs alongside chronic undernutrition.
Take home message
Current trends in national economic development, urbanisation, the globalisation of food systems and the adoption of “western” consumption patterns, indicate that the Indian Ocean Region is likely to face a significantly increased incidence of obesity and its associated health and productivity problems in coming years. This issue will confront both developed and developing countries in the region, but will place a heavier burden on developing countries that will not have the financial capacity to cope with related increases in NCDs. In these areas, the rapid rise in obesity rates is likely to contribute to a double burden, occurring alongside continuing problems with undernutrition and micronutrient deficiency. The projected exponential increase in obesity rates will moderate the pace of macroeconomic development and contribute to household poverty and malnutrition throughout the region.
Find out more:
Source: Future Directions International Pty Ltd, Dalkeith WA, Australia, www.futuredirections.org.au . Lauren Power is a Future Directions International research analyst for the Global Food and Water Crisis Research Program. Any opinions or views expressed in this paper are those of the individual author, unless stated to be those of Future Directions International.
Footnote:
The comments in this article about grains used in livestock production are not well researched and are too simplistic. It is important to note that if livestock, particularly ruminants, were not fed course grains, weather damaged food grains and food processing by-products, the world’s food grain stocks would be so high prices would be pushed below cost of production for most farmers supplying export markets. World food grains and feed grains are produced in approximately equal tonnages each year. If cropping land devoted to feed grains was diverted to grow food grains, stock piles would increase, in-storage damage would increase and grain prices would decline below cost of production. Low prices would divert some cropping farmers in major grain exporting nations into alternative enterprises such as livestock production, and renewable fuels. There would be even greater booms and busts in grain production and prices as farmers in major grain exporting nations such as Australia, South America and North America change enterprises in their search for profitability. – Patrick Francis